Lung-Sparing Pleurectomy With Decortication (P/D)
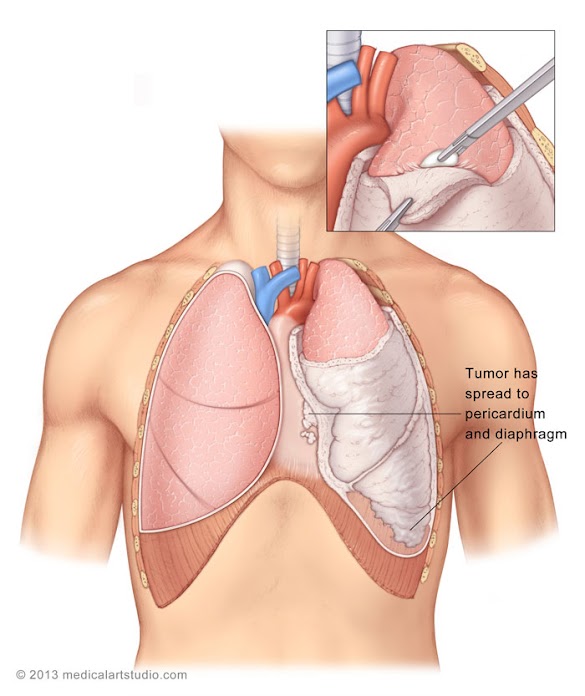
For some patients with pleural mesothelioma, pleurectomy/decortication (P/D) surgery is an aggressive but effective treatment option that can improve prognosis. This is a two-part surgical procedure that removes the thickened, diseased membranes lining the lung and chest wall (pleurectomy) along with visible tumors in the chest (decortication). The membrane enclosing the heart (the pericardial membrane) may also be removed if it appears similarly thickened and stiff, limiting the heart’s ability to efficiently pump blood.
Main Goals of Pleurectomy With Decortication:
- Serve as an alternative to the extrapleural pneumonectomy (EPP).
- ŸDelay mesothelioma progression by removing as much tumor bulk as possible.
- Improve breathing problems and pain caused by the typical thick fibrous bands and adhesions that encase the lung.
- Diminish or eliminate pressure from the excessive fluid that surrounds the lung in the majority of patients.
- Remove the membrane surrounding the heart (pericardial membrane) when its function is also affected.
- Patients facing surgery, and their families, are strongly encouraged to discuss the choice of surgery with their treatment team.
P/D is one of the two surgical approaches that account for the vast majority of procedures for malignant mesothelioma. The other is extra pleural pneumonectomy (EPP), a more radical procedure that, in contrast, requires removal of the lung and diaphragm on the cancerous side. There is no clear consensus about which procedure is best, and many experienced mesothelioma surgeons strongly favor one over the other. It is most likely that one is more effective than the other in different settings. Nonetheless, the proportion of patients undergoing P/D has been increasing through the last few decades. This trend is supported by numerous studies in the medical literature.
- As a more extensive surgical procedure, EPP is associated with consistently higher complication and mortality rates compared to P/D.
- For most patients, EPP does not result in sufficiently better results to justify the increased risks. In some settings P/D appears the better choice.
- When anti-cancer drug treatment and/or radiotherapy (multimodal or trimodal therapy) are combined with either procedure, survival is significantly longer than surgery alone.
- However, several studies have concluded that patients undergoing P/D are more likely to tolerate these additional treatments with better results.
The Pleurectomy/Decortication Procedure
P/D surgery combines two interrelated procedures done in a single session and only on the cancerous side. In most cases, P/D involves removal of the abnormal and constrictive pleural membranes, excision of all visible tumor tissue, and elimination of the accumulated excess fluid. P/D in any form is a major surgical procedure, but unlike EPP, it stops short of complete removal of the lung, pericardial membrane and diaphragm. The three basic steps are:
- Thoracotomy (Incision)
The P/D procedure requires inflation of the lung and a rather long incision to provide a sufficiently large opening into the chest cavity to visualize and remove as much abnormal tissue as possible. This incision usually begins in the mid back on the side of the tumor and then follows the rib curvature around to the same side of the chest wall. - Pleurectomy
In the pleurectomy part of the procedure, the diseased membrane lining the inside of the chest cavity (the parietal pleural membrane) is removed, exposing the underlying membrane covering the lung (visceral pleural membrane). - Decortication
In the decortication part, the tumor-laden visceral membrane is surgically separated and removed from the underlying lung. All other visible tumors are excised and, when appropriate, the heart’s covering membrane and any other similarly abnormal tissue are removed. Separation and removal of these membranes require a lot of time and surgical skill since they often adhere extensively to each other and the surfaces they cover.
Once completed, the incision is closed and at least one tube is inserted into the chest cavity in order to drain any fluids that accumulate thereafter. Since P/D is done under deep general anesthesia, the patient is unaware of the surgery and does not experience pain during the operation.
Alternative Method
Patients deemed ineligible for a P/D may opt for a video-assisted thoracoscopy for pleurectomy. This procedure is less invasive than P/D, but also is more limited. Using a small fiber optic camera and several other surgical instruments inserted through 3 very small incisions in the chest and back, it provides visualization of the pleural cavity, and can be used to obtain biopsies and perform a partial pleurectomy.
Recovery From Pleurectomy With Decortication
Pain following major surgery should be expected, and numerous options to control pain and discomfort are available. At the conclusion of surgery, one or more tubes will emerge from the chest in order to drain any accumulated fluid. During the early recovery period, breathing support is provided through a tube in the airway that is connected to a respirator. While the tube is in, you will be both unable to speak or ingest fluids. Before hospital discharge, the chest tube(s) will be removed as a bedside procedure that does not require further surgery.
On average, hospitalization lasts 1-2 weeks, followed by an additional 2-4 weeks before returning to normal activities.
Success Rates And Complications
Most estimates of mortality associated with P/D range from 1% to 5%; for the more extensive EPP surgery this is usually 2 to 3 times higher. P/D has a good track record for improving or relieving symptoms present before surgery. More than 80% of patients report satisfactory results for chest pain, excess fluid in the chest, cough, and breathing difficulties.
The causes of serious problems following P/D and EPP are essentially the same, but they occur more frequently after EPP. Between 5 – 15% of P/D patients will experience one or more serious complications compared to about 40-60% with EPP.
Complications that are commonly encountered are listed below along with estimates based on medical reports. For comparison, similar estimates are also provided for EPP.
Benefits and Life Expectancy
The main benefit of opting for a P/D is improved life expectancy. While the average life expectancy for patients with pleural mesothelioma is around a year with only about 5% of patients surviving for five years, patients who had a P/D experienced improved survival rates. In a study by Dr. Raja Flores, stage 1 mesothelioma patients experienced a survival rate of 40% after five years.
Another benefit of this surgery, which is often referred to as the lung-sparing or lung-saving option, is that the lung is not removed. In an EPP, the lung along with parts of the diaphragm and lining of the heart are also removed where tumors are present.
Dr. Robert Cameron, a known pioneer and leading doctor of P/D, believes “taking out a lung does harm and there is absolutely no benefit to the patient.” Dr. Sugarbaker, the creator of EPP, believes in both removing visible tumors and whatever is left “at the microscopic level.”
Ultimately, the right option is up to the patient and the advisement of their doctor based on eligibility and individual circumstances.
Sources:1. “Malignant Mesothelioma Treatment.” National Cancer Institute. N.p., n.d. Web. 29 Jan. 2016.
2. Lam, S. “Mesothelioma.” Mesothelioma.
3. “Malignant Mesothelioma.” Malignant Mesothelioma. Memorial Sloan Kettering Cancer Center.
4. Bhimji, S. Comprehensive & Technical Decortication.
5. Clinical trial. Combined P/D with chemotherapy and radiation therapy.
6. Clinical trial. Mesothelioma surgery following radiation therapy.
7 .Clinical trial. Chemotherapy followed by surgery and advanced radiation therapy.
8. Raja M. Flores (2008). Extrapleural pneumonectomy versus pleurectomy/decortication in the surgical management of malignant pleural mesothelioma: results in 663 patients. New York.
9. https://www.maacenter.org/treatment/surgery/pleurectomy-decortication/
Advertisement